80% of women develop fibroids by the time they are 50 years of age.¹
An emphasis on patient-centered care in uterine health has empowered women to raise their expectations on everything from education in diagnosis to innovations in treatment options. Reasons for recommended treatments are being questioned, and accuracy in predicted outcomes is expected.
Leiomyomas, also known as fibroids, represent the most common tumor of the reproductive tract,2 and women need to know what that means to their health. Many patients won’t know the difference between a fundal subserosal and a pedunculated submucosal fibroid, but they expect a thorough explanation.
Dr. Linda Bradley, Professor of Ob-Gyn & Reproductive Biology, Director of Center of Menstrual Disorders at Cleveland Clinic recommends women go to a practice that has multi-specialty expertise. She believes it is important for healthcare providers to be well versed in all areas of uterine health as well as current on modern fibroid treatment options.3
When it comes to selecting healthcare providers, women are looking beyond certifications. They want physicians who are committed to safe and effective modern treatments to meet their individual needs. When Dr. Bradley is asked for physician recommendations, she refers women to the American Association of Gynecologic Laparoscopists (AAGL). “These are people with special interests in minimally invasive surgery, which could include robot, hysteroscopy, or laparoscopy.”3
New technologies have elevated uterine health care by equipping physicians with safe and effective minimally invasive treatment options. Specifically, physicians have benefitted from innovations in devices to target FIGO PALM-COEIN Classification4 Type 0-2 submucosal fibroids, or those fibroids most associated with disruption to the endometrial layer causing Abnormal Uterine Bleeding (AUB), cramping, and infertility.
Modern medical technology has enabled healthcare providers to meet individual patient needs and achieve the best possible outcomes in ways that were not possible just a few years ago.
Breaking Down Diagnosis
Healthcare providers know that an accurate diagnosis is a critical first step in moving forward with the patient to determine the most appropriate treatments; however, many factors and challenges play into diagnosing leiomyomas.
Two common methods for diagnosing fibroids are transvaginal ultrasound (TVS) and saline-infused sonography (SIS). Physicians can achieve a better diagnostic value through SIS with sensitivity at 90% and a specificity of 79%. TVS offers 85% sensitivity but a specificity of only 56%.5
So why is TVS used in 70% of intrauterine diagnoses and SIS in only 20%? TVS is widely available and a relatively inexpensive method to evaluate uterine pathologies. Unfortunately, inaccurate interpretations may lead to misdiagnosis.6 Less common methods for fibroid diagnosis are the MRI or CT scan. While highly accurate, these methods are typically only used where multiple areas and/or conditions in the body mandate investigation.
Other procedures required for differential diagnosis of fibroids vs. other intrauterine pathology are endometrial tissue sampling and Dilation and Curettage (D&C). Endometrial tissue samples can diagnose endometrial intraepithelial hyperplasia, uterine polyps, and uterine cancer. When more information is needed, physicians recommend a Blind or Visual D&C, usually done in an operating room.
Another element that weighs and assists with leiomyoma diagnosis is the FIGO PALM-COEIN Classification. According to AAGL, best practice is to focus on several factors, including distinguishing leiomyomas from adenomyosis, confirmation of tumor location, as well the number and size(s).7
Regardless of the specific combination of the above methods used, an accurate diagnosis is critical when presenting the best treatment options to the patient.
Top Priorities of Patients
Providing the patient with a brief explanation prior to administering the examination may ease anxiety. Recommendations based on the patient’s individual needs may also bring comfort, especially if further examination or treatment is needed. Evidence suggests that involving patients in the decision-making process produces the best patient experience and outcome.8
According to the Department of Health, patient-centered care is seen as a critical aspect of quality of care. The National Academy of Medicine (NAM) defines patient-centered care as:
“Providing care that is respectful of, and responsive to, individual patient preferences, needs and values, and ensuring that patient values guide all clinical decisions.”9
Listening is key. Women not only want to ask questions, but they also want to be asked questions and to know that they are being heard. Increasingly, women arrive at the doctor’s office with at least some information in hand. They rely on healthcare providers to help them sort through their research and make an informed decision, beginning with the least invasive options. Physicians must tailor plans for individual patients on a case-by-case basis considering age, menopausal status, the patient’s desire to preserve fertility, and more. AAGL recognizes a minimally invasive approach as the first step in pain management where pelvic surgery is recommended, and most gynecologic surgery is now performed using minimally invasive approaches.10
Most gynecologic surgery is now performed using minimally invasive approaches. –AAGL
TECHNOLOGY & TREATMENT
Fibroid treatment options range from hormonal and non-hormonal drug therapies to hysterectomies. For some women, hormonal therapy can control symptoms, for others a hysterectomy is the right procedure. But what about cases in between? Doctors are no longer jumping from hormone medicine to hysterectomy as minimally invasive treatments have become a standard of care. This is partly due to the push for Minimally Invasive Gynecological Surgery (MIGS), which affords the patient a faster, less painful recovery, less risk of infection, a shorter hospital stay, and an earlier return to normal activities.11
Minimally invasive solutions for fibroid and polyp removal have evolved over the past 25 years, with the most significant improvements taking place in the past ten years. Prior to that, loop resection was the only method for hysteroscopic management of submucosal leiomyomas. This method never found significant adoption within the OB/GYN community, secondary to a significant surgical skill-set requirement, need for well-developed hand-eye-foot coordination, mandate for strict fluid monitoring, challenges associated with chip retrieval and a rather high risk profile.
It wasn’t until 2005 that side-channel cutting technologies were developed to simultaneously resect and evacuate the resected tissue; however, these technologies were primarily used for endometrial polyps, while patients with fibroids were still managed using more invasive surgical options. In 2010, the introduction of robotic-assisted laparoscopy had an unintended and negative effect of putting an even greater focus on hysterectomy procedures. Robotic-assisted tools advanced the precision but, at the same time, were responsible for a large spike in unnecessary hysterectomies, which could have been managed through a hysteroscopic approach.
In other words, there was little attention given to treatments for women experiencing symptomatic fibroids wanting to keep their uterus. The gynecologic community had little to no options in bridging the gap for women entering their 30s and 40s, where hormonal therapies were ineffective, and hysterectomies were excessive.
“One third of outpatient visits to the gynecologist are for AUB” –ACOG 12
Dr. Eugene Skalnyi, Vice President Medical Affairs at Minerva Surgical, and an OBGYN specializing in advanced operative GYN endoscopy and minimally invasive surgeries, explains, “The treatment pathway as a medical philosophy goes from non-invasive to more invasive. One should not start with the most invasive method, such as a hysterectomy. You go through the pathway to avoid major surgery, when appropriate.”
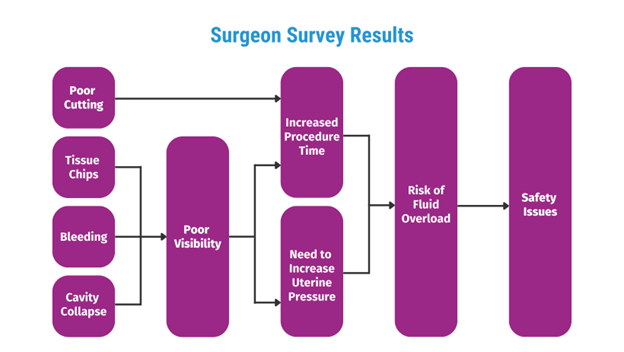
Side cutting, mechanical cutting devices were introduced in 2005 as a minimally invasive option of addressing intrauterine pathology. These devices effectively addressed the deficiencies of resectoscopic loop resection by automatic transport of the resected tissue, as well as the need for hypo- or non-ionic distention media. The skill set requirement for these novel procedures was significantly reduced, which allowed for their broad adoption by the Ob/Gyn community. In 2008, Minerva Surgical’s team of uterine health veterans looked at these systems holistically. They surveyed doctors to better understand the challenges and pain points and set out to develop a system that would remove most or all of the deficiencies of the existing solutions and provide a safe and effective option in one device. This is how the development of the Symphion® Operative Hysteroscopy System began.
During this research effort, physicians reported the following intraoperative challenges with the existing operative hysteroscopy systems available in 2008:
INTRAOPERATIVE CHALLENGES
- Poor Cutting – Manual blades are prone to dulling after some use, mandating replacement. This extends the procedure and anesthesia time and has a negative impact on the overall cost of the procedure.
- Tissue Chips – Loop Resection creates tissue chips that need to be removed, increasing the instances of device insertion and removal, thus increasing the risk of perforation.
- Cavity Collapse – Unintended drop in intrauterine pressure resulted in cavity collapse and poor visibility.
- Bleeding – When bleeding occurred when using older, non-resectoscopic tissue resection systems, it caused degradation of a surgeon’s visual field, because they lack the electrocautery tissue effect during tissue cutting and a specifically designed coagulation function to stop the bleeding. Lack of such critical function would leave the surgeon with only two options: 1) Raise intrauterine pressure to tamponade the bleeding (effectively increasing the rate of fluid absorption) or 2) Stop the case.A gap analysis was conducted and the Symphion system was designed to address shortcomings of existing tissue removal systems. The following list includes the surgeon’s list of concerns and how Minerva’s Symphion Operative Hysteroscopy System provides innovative solutions to overcome these challenges:
INNOVATIVE SOLUTIONS
- Poor Cutting – Symphion’s precision electrode allows for very precise and fast cutting, the rate of which is relatively independent of tissue hardness. Bi-Polar RF Plasma resection has the added benefit of allowing a 50X reduction the amount of thermal spread when compared to loop resection, reducing it from 2,000-3,000 microns to 40 microns on either side.
- Tissue Chips – During cutting, suction through Symphion’s bi-polar tissue removal device pulls the tissue into the resecting window and evacuates the tissue tips through the device, effectively eliminating presence of free-floating tissue chips in the uterine cavity.
- Visualization – An Independent Aspiration Function technology allows doctors to clear their visual field without running the resecting device, which is a significant safety improvement over the previous surgical solutions.
- Bleeding – Symphion’s fundamental design automatically controls bleeding and is secondary to the use of the bi-polar energy. When using the old-fashioned cold blade approach, the incised tissue instantaneously becomes an open gate for accelerated fluid absorption because of the breach in the integrity of the capillary bed, arterioles and venules. When a bi-polar RF approach implemented by Symphion is used to resect the target tissue, the small amount of localized heat, effectively produces a thin layer of ablated tissue, which effectively seals the capillary bed, arterioles, and venules, resulting in significant reduction of fluid absorption rate and bleeding during resection. In addition, if/when a larger caliber vessel is severed and resultant bleeding is not adequately controlled, a spot coagulation feature, directly unique to Symphion, can be used to apply bi-polar RF spot coagulation to the source of bleeding.
- Cavity Collapse – A pressure sensor mounted directly on the Symphion scope allows for direct intrauterine pressure monitoring and automatic flow adjustments resulting in quick, constant and accurate pressure control required for a quick, safe and convenient execution of the procedure as opposed to traditional systems that use an external machine with an observable lag-time.
- Fluid Overload – Symphion’s closed-loop Fluid Management Accessory uses just one 3L saline bag for the entire case. The fluid from the bag is advanced into the hysteroscope, into the uterine cavity, flows back through the resecting device, into the tissue catch, passes through a molecular filter, where it is cleaned to sterility, and is returned back into the saline bag. This approach reduces the load on the nursing personnel that no longer must hang new, heavy saline bags, and keep track of the number of bags used. Since no fluid is being drained out into any canisters, input/output calculation errors are reduced, as well as the subsequent cost of disposal of biohazard material. One can look at the saline bag and know exactly how much fluid was absorbed. When starting with the 3L bag, 500cc will be taken by the volume of the system (tubing, filter, other), leaving 2500cc of operational volume, which is representative of the maximum volume that can be lost, according to existing guidelines from ACOG and AAGL.13 This unique technological solution was implemented to reduce the chance of errors during fluid loss monitoring/calculation, eliminate the need for the use of multiple saline bags, reduce the level of stress in the OR, and reduce the overall cost of the procedure. Zero incidences of fluid overload have been reported when the Symphion system is used in accordance with the IFU.
Healthcare providers now have access to safe and effective minimally invasive treatment systems for Type 0-2 submucosal fibroids. According to Jerome Bauersfeld, Minerva Surgical’s Symphion Portfolio Brand Manager, “research shows that there are approximately 600,000 hysterectomies performed in the U.S. every year and it is estimated that approximately 200,000 of those were cases that could have been treated in less invasive and organ-preserving ways.”
As of 2020, Minerva Surgical has the most comprehensive suite of minimally invasive intrauterine treatment solutions available to healthcare providers. The company’s two distinct tissue resection solutions include Symphion for hysteroscopic removal of fibroids and polyps, and Resectr for gynecologists treating polyps in an office setting. The Minerva ES and Genesys HTA endometrial ablation systems complement Minerva Surgical’s complete product line to treat the most common causes of Abnormal Uterine Bleeding (AUB) in most uterine anatomies.
Healthcare Provider & Physician Resources
The best thing healthcare providers and physicians can do is 1) look for the most current research and data and 2) listen to their patients.
Healthcare professionals should look for complete systems with a support team aiding physicians along the entire patient journey from education to outcome. Minerva Surgical has a resource center with instructional videos, comparison charts, physician testimonials, patient discussion guides, clinical data and studies, and reimbursement guides.
Make sure to visit the Symphion information page to see the system in action. The following quick links may also assist you in your research:
Video: Symphion system removing submucosal leiomyomas
AAGL Practice Report: Practice Guidelines for the Diagnosis and
Management of Submucous Leiomyomas: https://www.aagl.org/wp-content/uploads/2013/03/aagl-Practice-Guidelines-for-the-Diagnosis-and-Management-of-Submucous-Leiomyomas.pdf
Resources for Hospitals and Physicians: https://minervasurgical.com/resource-library/
INDICATIONS: The Symphion® System is intended to distend the uterus by filling it with saline to facilitate viewing with a hysteroscope during diagnostic and operative hysteroscopy and provide fluid management through the closed loop recirculation of filtered distension fluid. It is also intended for resection and coagulation of uterine tissue such as intrauterine polyps and myomas using a bipolar resecting device. For a complete list of contraindications, potential adverse events, warnings and precautions, visit www.minervasurgical.com/safety
CAUTION: Federal law (USA) restricts this device to sale by or on the order of a physician. Rx only. They physician using the system must be trained in hysteroscopy. Prior to use, consult the Instructions for Use and/or Operators Manual
REFERENCES:
- Office on Women’s Health.( 2021 ) Uterine Fibroids. Womenshealth.gov. Accessed August 16, 2022. https://www.womenshealth.gov/a-z-topics/uterine-fibroids Updated April 1, 2019.
- UCLA Health.( 2022 ) What are Fibroids? Uclahealth.org. Accessed September 15, 2022. https://www.uclahealth.org/medical-services/fibroids/what-are-fibroids#:~:text=Uterine%20fibroids%20are%20the%20most,between%20periods%20and%20pelvic%20pain
- The Fibroid Foundation.( February 4, 2013) MEDICAL SPOTLIGHT: Dr. Linda Bradley, Director of The Fibroid and Menstrual Disorders Center at The Cleveland Clinic. Fibroidfoundation.org. Accessed August 16, 2022. https://www.fibroidfoundation.org/2013/02/04/medical-spotlight-dr-linda-bradley-director-of-the-fibroid-and-menstrual-disorders-center-at-the-cleveland-clinic/
- Munro MG, Critchley HO, Broder MS, Fraser IS; FIGO Working Group on Menstrual Disorders. FIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. Int J Gynaecol Obstet. 2011;113(1):3-13.
- National Library of Medicine, PMCID: PMC3992420 PMID: 24753775 Exp Med. 2014; 7(3): 764–769. ( Published online 2014 Mar 15 ) Comparison of transvaginal ultrasonography and hysteroscopy in the diagnosis of uterine pathologies. Accessed August 16, 2022. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3992420/
- Zhang M, Wasnik AP, Masch WR, et al.( May 6, 2018 ) Transvaginal ultrasound shear wave elastography for the evaluation of benign uterine pathologies: a prospective pilot study. Journal of Ultrasound in Med. 2019;38:149–55. Wiley Online Library. Accessed August 16, 2022. https://onlinelibrary.wiley.com/doi/10.1002/jum.14676
- The Journal of Minimally Invasive Gynecology.( 2012 ) AAGL Practice Report: Practice Guidelines for the Diagnosis and Management of Submucous Leiomyomas aagl.org. Accessed August 26, 2022. https://www.aagl.org/wp-content/uploads/2013/03/aagl-Practice-Guidelines-for-the-Diagnosis-and-Management-of-Submucous-Leiomyomas.pdf
- National Library of Medicine, PMCID: PMC3964421 PMID: 24719703 ( Published online 2014 Jan 5 ) Patient Involvement in Health Care Decision Making: A Review. Accessed September 15, 2022. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3964421/
- Ignatius Bau, Robert A. Logan, Christopher Dezii, Bernard Rosof, Alicia Fernandez, Michael K. Paasche-Orlow, and Winston F. Wong( February 11, 2019 )Patient-Centered, Integrated Health Care Quality Measures Could Improve Health Literacy, Language Access, and Cultural Competence. National Academy of Medicine. Nam.edu. Accessed August 26, 2022. https://nam.edu/patient-centered-integrated-health-care-quality-measures-could-improve-health-literacy-language-access-and-cultural-competence/?gclid=CjwKCAjw3qGYBhBSEiwAcnTRLisUSuNOENaQSCSCxAwi1og3TEslmkPGr8KMYMwBcs2slZSk25OY1xoCboEQAvD_BwE
- Rebecca Stone, MD, MS, Erin Carey, MD, Amanda N. Fader, MD, Jocelyn Fitzgerald, MD, Lee Hammons, MD, Alysha Nensi, MD, Amy J. Park, MD, Stephanie Ricci, MD, Rick Rosenfield, MD, Stacey Scheib, MD, and Erica Weston, MD( August 13, 2020 )Enhanced Recovery and Surgical Optimization Protocol for Minimally Invasive Gynecologic Surgery: An AAGL White Paper. The Journal of Minimally Invasive Gynecology. aagl.org. Accessed August 16, 2022. https://www.aagl.org/wp-content/uploads/2020/10/PIIS155346502030385X.pdf
- John Hopkins Medicine.( 2022 ) hopkinsmedicine.org. Accessed August 16, 2022. https://www.hopkinsmedicine.org/gynecology_obstetrics/specialty_areas/gynecological_services/treatments_services/minimally-invasive-gyn-surgery/index.html#benefits
- The American College of Obstetricians and Gynecologists.( 2022 )ACOG Clinical. acog.org. Accessed August 16, 2022. https://www.acog.org/clinical/clinical-guidance/practice-bulletin/articles/2012/07/diagnosis-of-abnormal-uterine-bleeding-in-reproductive-aged-women
- The Journal of Minimally Invasive Gynecology. ( 2013) AAGL Practice Report: Practice Guidelines for the Management of Hysteroscopic Distending Media (Replaces Hysteroscopic Fluid Monitoring Guidelines. J Am Assoc Gynecol Laparosc. 2000;7:167–168.) aagl.org. Accessed August 16, 2022. https://www.aagl.org/wp-content/uploads/2013/03/aagl-Practice-Guidelines-for-the-Management-of-Hysteroscopic-Distending-Media.pdf
K0177 Rev. A
